Pradeep Attaluri, Shady Elmaraghi, Claudia Vilela Casaretto, Brian Gander, Courtney Morgan, Amgad Hanna
Abstract
Background
Brachial artery pseudoaneurysms (PSAs) are a rare complication of trauma and medical intervention, estimated to constitute 0.3–0.7% of all PSAs. Although neurologic symptoms are common in patients undergoing hemodialysis, direct nerve compression by large PSAs is rare.
Case Description
We report a case of median nerve compression by a brachial artery PSA treated by PSA resection and distal nerve transfer of the extensor carpi radialis brevis nerve to the anterior interosseous nerve.
Conclusion
This case illustrates the successful use of distal nerve transfers for the treatment of median neuropathy secondary to brachial PSA. In addition, this case highlights the importance of imaging before any exploratory nerve surgery in the setting of a mass and/or prior vascular procedure. Embarking on a nerve release/ repair surgery in the absence of a vascular surgeon would be disastrous.
Introduction
Brachial artery pseudoaneurysms (PSAs) are a rare complication of trauma and medical intervention, estimated to constitute 0.3–0.7% of all PSAs.[1] Literature on noninfectious PSAs associated with hemodialysis access is limited to case studies and small case series. Chemla et al. report an overall incidence of 4.5% in a population of patients with arteriovenous fistulas for hemodialysis access.[2] Although neurologic symptoms are common in patients undergoing hemodialysis, direct nerve compression by large PSA is rare.[3-10] We report a case of median nerve compression by a brachial artery PSA treated by PSA resection and distal nerve transfer.
Case Presentation
A 69-year-old male presented to our multidisciplinary brachial plexus clinic with severe proximal median neuropathy causing paresthesia in the median nerve distribution, benediction hand [Figure 1a], and weakness of his extrinsic finger flexors, flexor digitorum profundus (FDP) to his index finger, flexor pollicis longus (FPL), and median innervated hand intrinsics. His past medical history was significant for end-stage renal failure requiring dialysis through a right brachiocephalic fistula. Nine months prior, during an attempt to cannulate his fistula for dialysis access, he experienced significant pain and paresthesia in the median nerve distribution. Initially, he did not have symptoms of weakness. Over three months, he experienced progressive numbness and weakness in the hand.
Figure 1:

(a) Preoperative presentation of the patient showing physical examination consistent with benediction hand. (b) Preoperative photograph showing compressible swelling in the upper arm. A positive Tinel’s sign over the expected course of the median nerve in the upper arm was also noted to be present.
On initial physical examination, he demonstrated Medical Research Council (MRC) Grade 4/5 pronator teres (PT) strength, 0/5 FPL, 0/5 abductor pollicis brevis (APB), 0/5 flexor digitorum superficialis (FDS), 0/5 FDP to index finger, and 4/5 FDP to the remaining fingers. Sensory examination was significant for diminished sensation to light touch in the palmar cutaneous branch distribution and 10–14 mm static two-point discrimination in the median nerve distribution of the fingers. In addition, he had a positive Tinel sign and sensory collapse test over the carpal tunnel and PT. He was noted to have compressible swelling over the medial upper arm [Figure 1b] with a positive Tinel sign over the expected course of the median nerve proximal to the elbow.
Electrodiagnostic studies were obtained and confirmed severe median neuropathy proximal to the takeoff of the PT. These electrodiagnostic findings suggested a severe median neuropathy localizing proximal to the elbow. In addition, low compound muscle action potentials (CMAPs) and absent sensory nerve conduction suggested some degree of axonal injury.
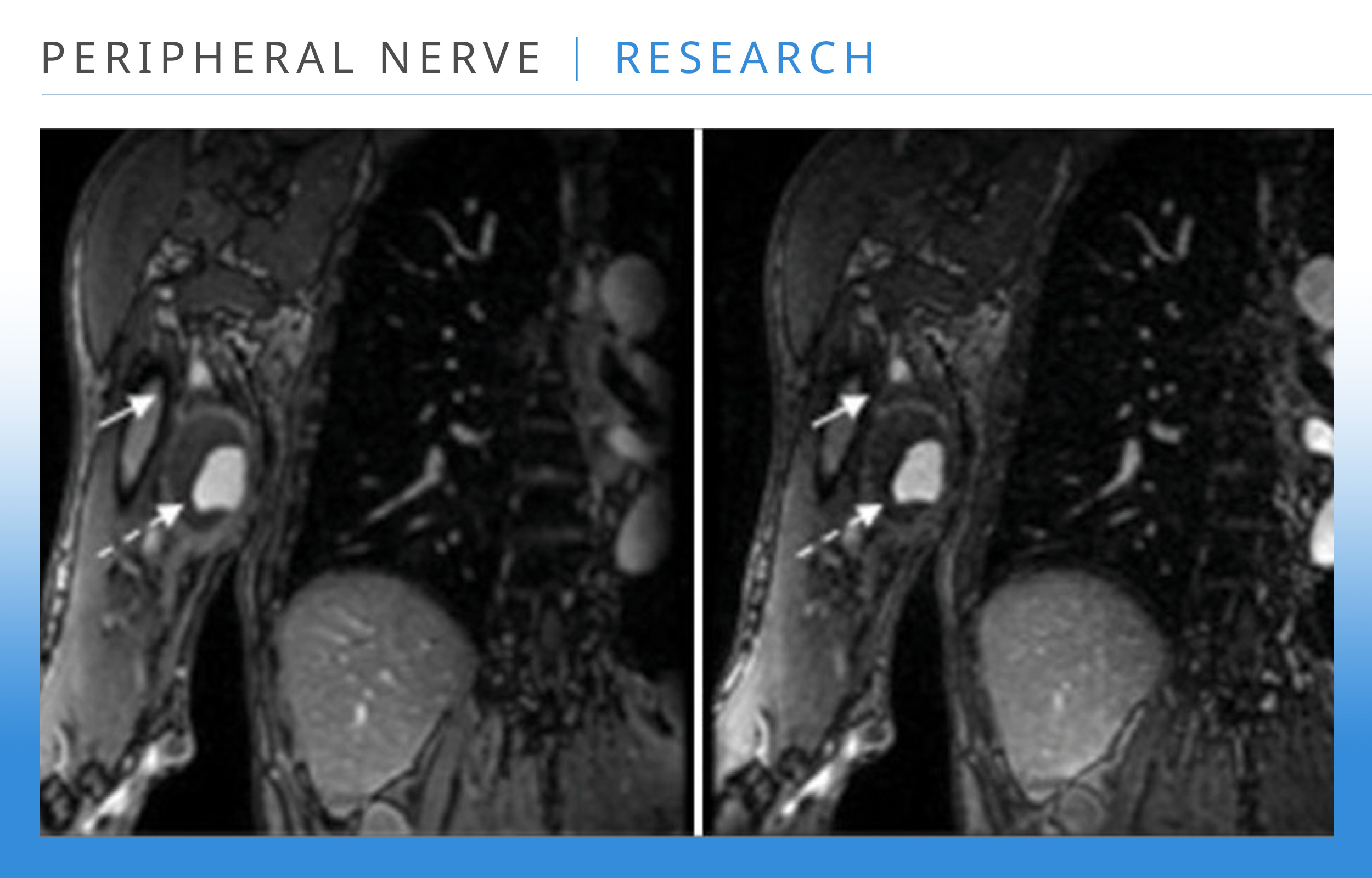
Magnetic resonance imaging and magnetic resonance angiography were also obtained and showed a 4.6 cm × 4.2 cm × 6.7 cm mass, likely a PSA within the brachial artery, compressing the median nerve [Figure 2].
Figure 2:
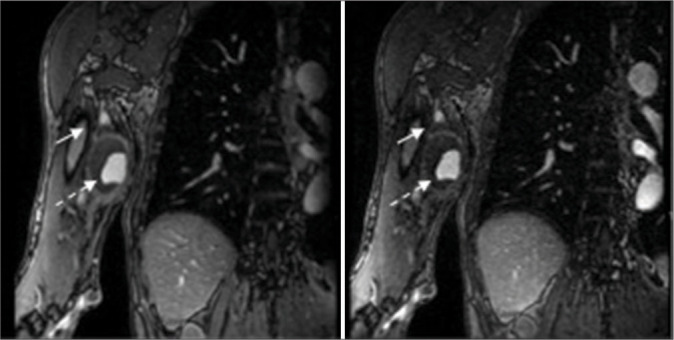
A 4.2 × 5.2 × 6.7 cm mass located at the level of the mid humeral shaft abutting the medial aspect of the brachial artery (dashed arrow). The median nerve (solid arrow) demonstrates thickening, edema, and abnormal enhancement at the level of the mass through the distal humerus. The median nerve is compressed as it contours the anterior margin of the mass.
In conjunction with vascular surgery who planned to resect and repair the brachial artery PSA, we decided to proceed with decompression of the median nerve in the upper arm, forearm, and carpal tunnel, along with distal extensor carpi radialis brevis (ECRB) to anterior interosseous nerve (AIN) transfer to restore pinch. Intraoperatively, we were able to successfully resect and reconstruct the brachial artery PSA [Figures 3a and b]. The median nerve in the upper arm was noted to have significant circumferential adhesions extending distally to the elbow. Circumferential release of the median nerve was performed in the upper arm, at the PT, and distally at the carpal tunnel. After the release of adhesions, the fascicles appeared scarred but in continuity. Nerve action potentials were negative. However, due to the long segment of unhealthy-looking nerve, it was decided to do the nerve transfer and not cut and graft since the grafts would have been longer than 12 cm. In addition, distal ECRB to AIN transfer was performed with coaptation using an 8-0 nylon suture and nerve wrap [Figure 4].
Figure 3:
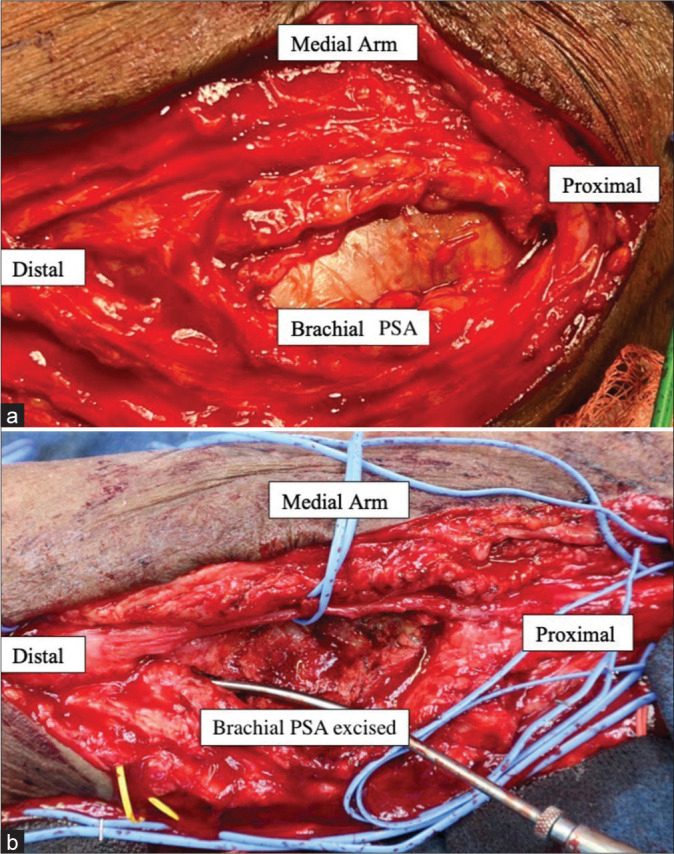
Intraoperative photograph showing the proximal extensor carpi radialis brevis (ECRB) branch with a tension-free coaptation to the anterior interosseous nerve (AIN) with nerve wrap.
At 1-year follow-up, the patient has regained some function of the median nerve. On physical examination, he was found to have MRC grade 2/5 FPL strength, FDS 2/5, FDP to the index 2/5, and APB 0/5. On transcutaneous electrical nerve stimulation examination, he notes sensation in the palmar cutaneous branch distribution to be 60% of the contralateral side and sensation in the fingers in the median nerve distribution around 40% of the contralateral side. He is currently planning to undergo opponensplasty to restore thumb opposition.
Discussion
Previous studies reporting on the treatment of arterial PSA causing nerve compression have focused on decompression by surgical management of the PSA. Papadopoulos et al. reported two cases of median neuropathy associated with a brachial artery aneurysm in which neurological symptoms completely resolved after resection of the compressive PSA.[7] Other case studies also reported complete resolution of symptoms with resection of the PSA alone.[4,8,9] However, these studies report on cases that were treated acutely (<3 months of symptoms), allowing for decompression alone as the sole modality of treatment. We report a case of delayed presentation of severe proximal median neuropathy with evidence of axonal loss on electrodiagnostic studies. In this case, it is unclear whether axonal loss was induced by prolonged unrecognized compression or by direct injury during dialysis access. However, we elected to perform distal nerve transfers due to the low likelihood of spontaneous motor recovery after this prolonged period of denervation and the distance from the level of injury to the target. This is further supported by the lack of recovery of the median innervated hand intrinsics one year after PSA resection and median nerve release.
Conclusion
To our knowledge, this is the first reported case of the successful use of distal nerve transfers for the treatment of median neuropathy secondary to brachial PSA. In addition, this case illustrates the importance of imaging before any exploratory nerve surgery in the setting of a mass and/or prior vascular procedure. Embarking on a nerve release/ repair surgery in the absence of a vascular surgeon would have been a disaster in this case.